Introduction: Acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL) are the most aggressive group of hematologic malignancies (Pulte et al, 2020) and will be responsible for approximately 12,700 deaths in the U.S. during 2023(Seiger et al,2023). Improved overall survival (OS) has been observed in the past decades in both diseases, but high mortality in the Intensive Care Unit (ICU) persists, which may prevent ICU admission of those patients. We aimed to review the literature on mortality data and survival predictors of patients with acute leukemia (AL) admitted to the ICU.
Methods: Embase, Pubmed and Cochrane databases were searched for articles published from January of 2005 to December of 2020. Due to OS improvement of patients with AML, we only included studies published as of 2005 (Percival et al, 2015). Editorials, case reports and small case series were excluded.
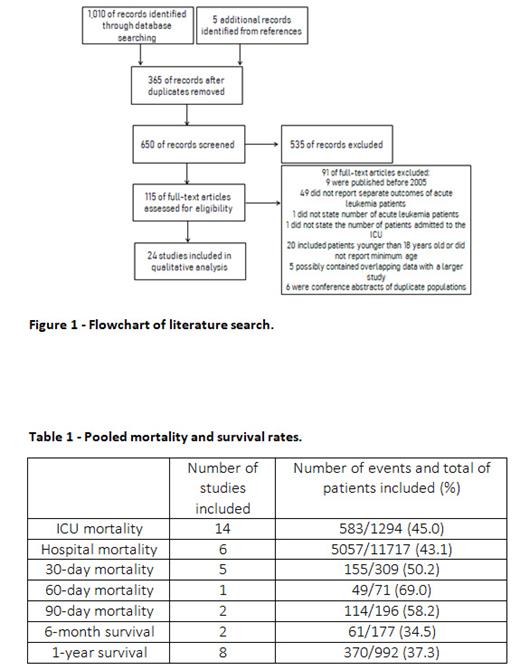
Results: Initial search revealed 1,015 manuscripts from database and references, 650 were screened and 115 were fully assessed, for which 24 met eligibility criteria (Figure 1). A total of 13,350 patients were included in the review. Median age was 54.8 years and 57.3% of patients were male. AML represented the majority of diagnoses (98.2%).Two studies included only newly diagnosed patients, 1 study only included patients with relapsed disease and the rest (N=21) included subjects regardless of the AL status. Only 0.7% of patients had a history of hematopoietic stem cell transplantation . 81.9% of patients required mechanical ventilation, 25.3% needed renal replacement therapy, and 65.9% used vasopressors in studies data was available. Median SOFA score in the first 24h of ICU admission was 10.85 . Pooled ICU mortality and hospital mortality were 45.0% and 43.1%, respectively; 58.2% of patients were deceased at 90-day mark (Table 1). The 12 months OS was 37.3%. Higher SOFA score, need for mechanical ventilation, sepsis, vasopressor use, and age greater than 60 years were the most common predictors of ICU, hospital and 90-day mortality. Relapsed or refractory status of underlying AL was the most significant risk factor for long-term mortality.
Conclusions: Our systemic review showed that ICU mortality in patients with AL was 45.0%, which represents a survival improvement compared to prior studies on patients with hematological malignancies, where ICU mortality could be as high as 69% (Ashkenazi et al, 1986). Predictors of ICU mortality were closely related to the severity of acute illness rather than malignancy status. We acknowledge that our patient population was mostly comprised of AML cases and the majority of the original studies included a small number of patients with AL with exception of one large study (Halpern et al, 2017).
Disclosures
Sandoval-Sus:ADC Therapeutics: Other: Advisory Board; BeiGene: Other: Ad Board; Genentech: Other: Ad Board; Abbvie: Other: Ad Board; Genmab: Other: Advisory Board; Janssen: Other: Advisory Board; Seagen: Other: Advisory Board, Speakers Bureau; Incyte: Other: Advisory Board; MassiveBio: Other: Advisory Board; TG Therapeutics: Other: Advisory Board.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal